Mondor’s Disease is a rare problem with blood vessels that leads to inflammation and blood clots in the surface veins. It can happen in different parts of the body, but it’s often called penile Mondor’s disease (PMD) when it affects the penis. PMD typically happens because of penis injury or intense sexual activity, sometimes with a genetic factor.
Doctors can diagnose Mondor’s Disease, including PMD, by examining the affected area and using ultrasound imaging. Although the condition usually gets better by itself in four to six weeks, treatment focuses on easing pain and inflammation.
Even though PMD is not common, with fewer than 400 cases reported worldwide, it’s important to understand its symptoms, causes, and treatment options for early detection and care.
Key Takeaways:
- Mondor’s Disease is a rare vascular condition characterized by thrombophlebitis in the superficial veins.
- PMD, also known as penile Mondor’s disease, primarily occurs due to trauma to the penis or vigorous sexual activity.
- The diagnosis of Mondor’s Disease is made through physical examination and ultrasound imaging.
- Treatment for Mondor’s Disease focuses on supportive care to relieve pain and inflammation.
- Complications are rare, but individuals should be aware of the risk factors and seek medical attention if necessary.
What is Mondor’s Disease?
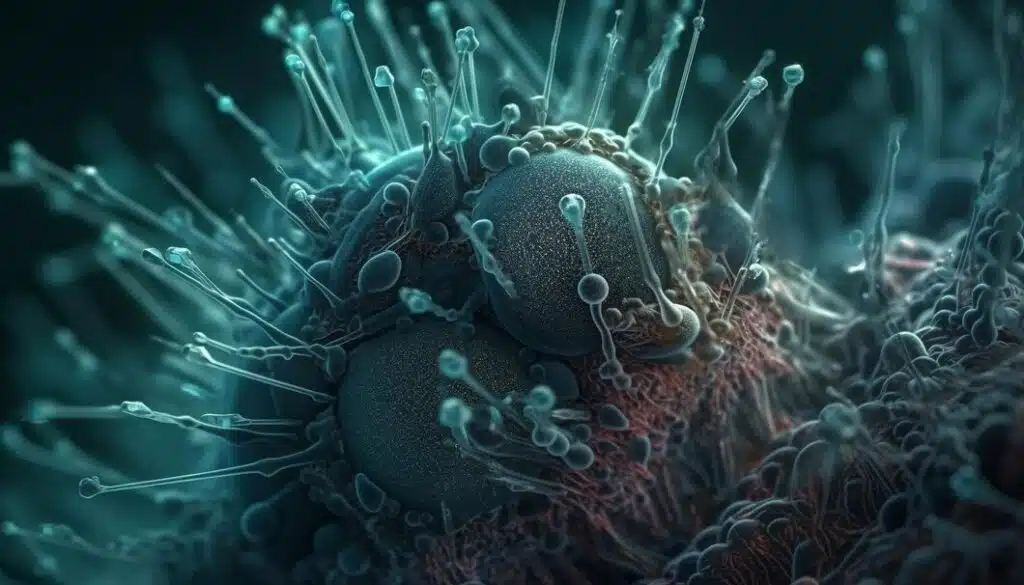
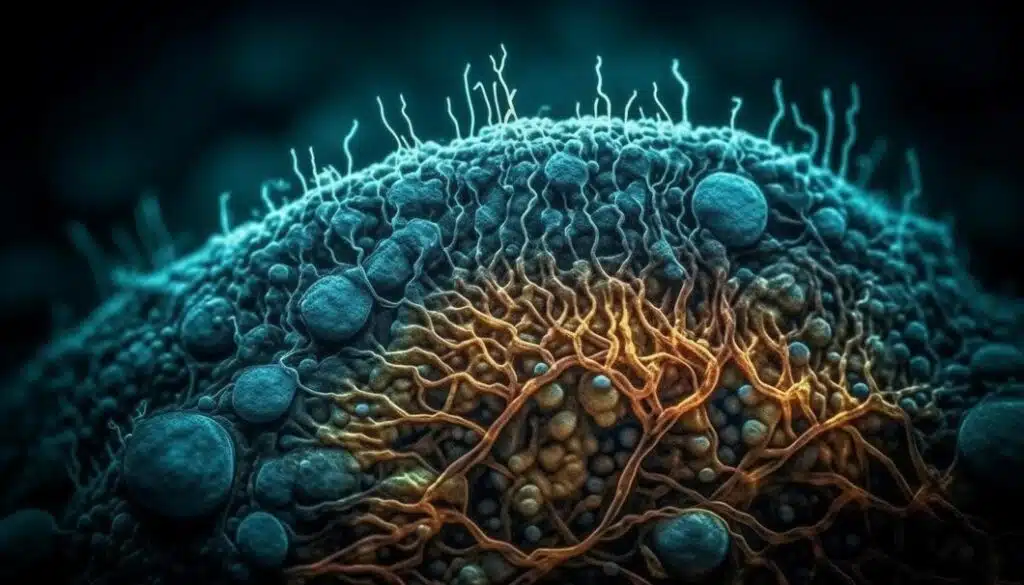
Mondor’s Disease, first described by Henri Mondor in 1939, is a rare vascular condition characterized by thrombophlebitis of the chest wall and breast, extending to the arm and penis in some cases. Thrombophlebitis is an inflammatory process that leads to the formation of blood clots in the veins. Mondor’s Disease is believed to have a genetic origin and can occur after trauma to the penis or vigorous sexual activity.
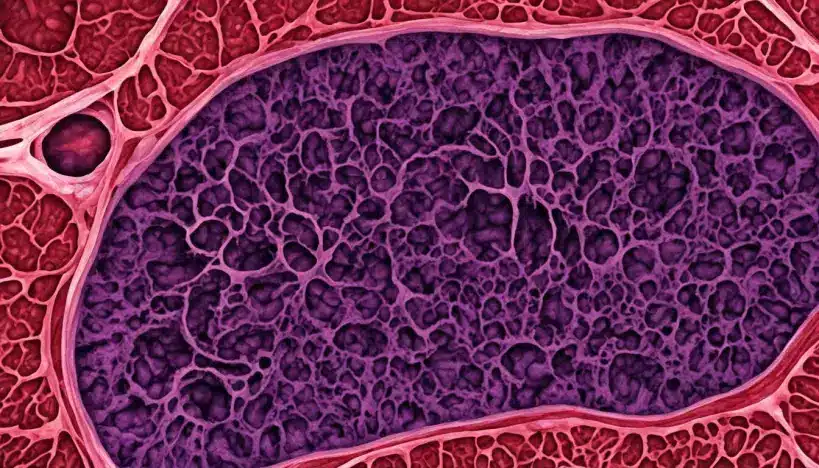
Penile Mondor’s Disease (PMD) is a manifestation of Mondor’s Disease and typically affects the superficial dorsal vein of the penis. PMD can result in pain, swelling, and a hardened vein on the top of the penis, making it easily identifiable through physical examination.
To give you a better understanding of Mondor’s Disease, let’s take a look at the following table that compares different characteristics of this condition:
| Feature | Mondor’s Disease | Penile Mondor’s Disease (PMD) |
|---|---|---|
| Etiology | Genetic origin, trauma, hypercoagulable state | Trauma, genetic predisposition |
| Location | Chest wall, breast, arm, penis | Superficial dorsal vein of the penis |
| Symptoms | Pain, swelling, hardened vein | Pain, swelling, hardened vein |
| Diagnosis | Physical exam, ultrasound | Physical exam, ultrasound |
| Treatment | Supportive care, topical creams | Supportive care, topical creams |
| Complications | Deep vein thrombosis | None reported |
This table provides a quick comparison between Mondor’s Disease and its specific manifestation, penile Mondor’s Disease. Understanding the similarities and differences can help in recognizing and effectively managing these conditions.
Now that you have an overview of Mondor’s Disease, the following section will delve into the specific symptoms experienced by individuals affected by this condition.
Symptoms of Mondor’s Disease

Mondor’s Disease, including penile Mondor’s disease, can present with a variety of symptoms. The most common ones include:
- Pain: Patients with Mondor’s Disease often experience pain, especially around the affected area. In penile Mondor’s disease, the first sign is typically a palpable hardening of part of the dorsal vein on top of the penis.
- Swelling: Swelling, particularly in the affected vein, is another noticeable symptom. It can contribute to a firm and enlarged area.
- Edema: The condition may also cause localized edema, characterized by fluid buildup in the tissues, leading to increased swelling.
In addition to these primary symptoms, individuals with penile Mondor’s disease may experience pain during an erection, difficulty urinating, and superficial reddening of the skin (erythema). These symptoms are often triggered by a prior event, such as prolonged and vigorous sexual activity.
It is essential to note that symptoms can vary from person to person. Some individuals may experience mild discomfort, while others may have more pronounced pain and swelling.
Consult a healthcare professional for an accurate diagnosis and appropriate management if you suspect you have symptoms of Mondor’s Disease.
Mondor’s Disease Symptoms Overview:
| Symptoms | Frequency |
|---|---|
| Pain | Common |
| Swelling | Common |
| Edema | Common |
| Pain during an erection | Varies |
| Difficulty urinating | Varies |
| Superficial reddening of the skin (erythema) | Varies |
Causes of Mondor’s Disease
Mondor’s Disease, including penile Mondor’s disease, can have several causes. While the exact cause is not fully understood, there are a few factors that are believed to contribute to its development.
- Trauma: Mechanical trauma to the penis is a common cause of Mondor’s Disease. This can include injury during sexual activity, vigorous masturbation, or accidental trauma during daily activities.
- Genetic Predisposition: Certain gene mutations have been associated with an increased risk of developing Mondor’s Disease. Individuals with a genetic predisposition may have a higher likelihood of experiencing the condition.
- Underlying Conditions: Mondor’s Disease can be secondary to various diseases, infections, or surgeries that affect the penis. Additionally, individuals with a hypercoagulable state or thrombophilia, which is the tendency to form blood clots, may be more susceptible to developing the condition.
It is important to note that while these factors may increase the risk of Mondor’s Disease, not everyone who experiences them will develop the condition. The exact interplay between these causes and the development of Mondor’s Disease requires further research.
Diagnosis of Mondor’s Disease
To find out if someone has Mondor’s Disease, especially penile Mondor’s disease, doctors use a combination of physical examination and imaging tests. During the physical exam, the doctor checks the affected area carefully. They look for classic signs, like a hard vein on top of the penis that can be felt. This is an important clue that Mondor’s Disease might be the issue.
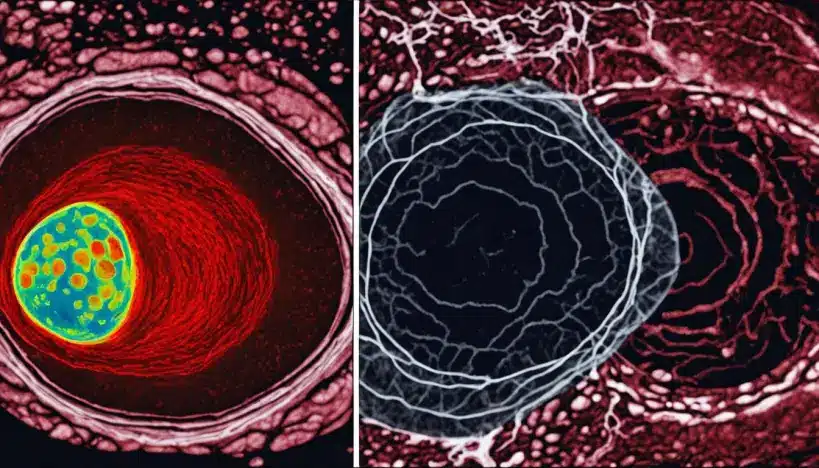
For further confirmation, doctors often use imaging tests, mainly ultrasound. Ultrasound is a painless and non-invasive procedure that uses sound waves to create a picture of the area in question. In Mondor’s Disease cases, a special type of ultrasound called color Doppler ultrasound is helpful. It lets the doctor see the blood flow in the veins, helping to tell Mondor’s Disease apart from other conditions.
The ultrasound results may show a tube-like structure in the affected vein that doesn’t compress easily and appears darker on the image. This supports the diagnosis of Mondor’s Disease and gives crucial information for managing the condition properly.
Diagnostic Criteria for Mondor’s Disease
In order to diagnose Mondor’s Disease accurately, the following diagnostic criteria are often considered:
- Physical examination revealing a palpable hardened vein on top of the penis
- Ultrasound findings of a non-compressible, hypoechoic tubular structure corresponding to the affected superficial vein
- Exclusion of other similar conditions through a thorough evaluation
Clinical Pearls
Color Doppler ultrasound is a valuable tool in the diagnosis of Mondor’s Disease, as it allows for the visualization of blood flow within the affected veins.
| Diagnostic Methods | Advantages | Disadvantages |
|---|---|---|
| Physical Examination | – Non-invasive – Can be performed at the bedside | – Subjective interpretation – Limited to surface findings |
| Ultrasound | – Non-invasive – Provides visualization of the affected veins – Can assist in ruling out other conditions | – Operator-dependent – Requires specialized equipment |
Treatment of Mondor’s Disease
The treatment of Mondor’s Disease, including penile Mondor’s disease, focuses on supportive care to alleviate pain and reduce inflammation. The primary goal is to promote the body’s natural healing process. Treatment options for Mondor’s Disease may include:
1. Supportive Care:
Symptomatic relief can be achieved through supportive care measures. This may involve applying warm compresses to the affected area, which can help improve blood circulation and reduce discomfort. Nonsteroidal anti-inflammatory drugs (NSAIDs) may also be recommended to relieve pain and inflammation.
2. Topical Creams:
Topical creams containing heparin or other anti-inflammatory agents may be prescribed to help alleviate symptoms and reduce inflammation. These creams can be applied directly to the affected area to provide localized relief.
3. Abstinence from Sexual Activity:
Abstaining from sexual activity until the symptoms of Mondor’s Disease resolve is crucial. Engaging in sexual activity may aggravate the inflammation and delay the healing process. It is important to prioritize rest and allow the body time to recover.
4. Surgical Intervention:
In rare cases where conservative measures are not effective, surgery may be considered as a treatment option for Mondor’s Disease. Surgical interventions, such as thrombectomy or resection, may be performed to remove the blood clot and affected vein. This can help alleviate symptoms and promote healing.
It is important to consult with a healthcare professional for a personalized treatment plan based on the severity and specific characteristics of Mondor’s Disease. While the condition is usually self-limiting and resolves within a few weeks, seeking medical guidance can ensure appropriate management and minimize the risk of complications.
Complications of Mondor’s Disease

Mondor’s Disease, including penile Mondor’s disease, is typically a self-limiting condition that resolves on its own without complications. However, in rare cases, there is a small risk of developing deep vein thrombosis (DVT), which involves the formation of blood clots in deeper veins.
DVT can be a serious condition that requires medical attention. It is important to monitor for any signs or symptoms of DVT, such as persistent pain, swelling, redness, warmth, or tenderness in the affected area.
If you experience any of these symptoms or are concerned about the possibility of DVT, it is crucial to seek prompt medical evaluation to rule out this complication. Your healthcare provider can perform diagnostic tests, such as ultrasound or venography, to confirm the presence of deep vein thrombosis.
| Complications of Mondor’s Disease | Description |
|---|---|
| Deep Vein Thrombosis (DVT) | A condition characterized by the formation of blood clots in deeper veins, which can be potentially dangerous. Symptoms include pain, swelling, redness, warmth, or tenderness in the affected area. |
If deep vein thrombosis is diagnosed, your healthcare provider will recommend appropriate treatment, which may include blood thinners, compression stockings, or, in rare cases, surgical intervention.
It is important to note that while complications are rare, it is crucial to be aware of the potential risks associated with Mondor’s Disease and seek timely medical attention if any concerning symptoms arise.
Prevention and Risk Factors of Mondor’s Disease
While there are no specific preventive measures for Mondor’s Disease, it is important to be aware of the risk factors that may increase the likelihood of developing this rare vascular condition.
One significant risk factor is a genetic predisposition. Individuals with a family history of Mondor’s Disease may have an increased susceptibility to the condition. In such cases, it is crucial to monitor for any potential symptoms and seek medical attention promptly.
Another risk factor is a history of trauma or injury. Trauma to the affected area, such as the breast, chest wall, or penis, can cause inflammation and lead to the development of Mondor’s Disease. It is essential to take precautions to prevent injuries in these areas, especially during activities that may pose a higher risk of trauma.
Furthermore, individuals with a hypercoagulable state, a condition characterized by increased blood clotting, may be more susceptible to developing Mondor’s Disease. Certain underlying conditions and medications can contribute to a hypercoagulable state. It is important to discuss any concerns or medical history with a healthcare professional to assess the individual risk.
Being aware of these risk factors can help individuals take the necessary precautions and seek appropriate medical care if any symptoms of Mondor’s Disease occur.
Key Prevention and Risk Factors:
- Genetic predisposition
- History of trauma or injury
- Hypercoagulable state
Mondor’s Disease in Women and Men
Mondor’s Disease, including penile Mondor’s disease, can affect both women and men. However, it is more commonly reported in women. The exact prevalence of Mondor’s Disease in the general population is unknown due to the rarity of the condition and underreporting. It is important for individuals of all genders to be aware of the symptoms and risk factors associated with Mondor’s Disease.
Prevalence of Mondor’s Disease in Women and Men
The prevalence of Mondor’s Disease varies among different populations. While there is limited data on the exact prevalence in women and men, studies suggest that women are more commonly affected by this condition than men. However, it is important to note that the rarity of Mondor’s Disease makes it difficult to determine the precise prevalence rates.
Gender Differences in Symptom Presentation
Mondor’s Disease may present with similar symptoms in both women and men, including pain, swelling, and the palpable hardening of veins. However, the affected areas may differ between genders. In women, the chest wall and breast are often involved, while in men, the penile area is frequently affected.
Risk Factors for Mondor’s Disease
While anyone can develop Mondor’s Disease, certain risk factors may increase the likelihood of its occurrence. These risk factors include:
- Genetic predisposition: Some individuals may have a genetic susceptibility to developing Mondor’s Disease.
- Trauma: Trauma to the chest wall, breast, or penile area can contribute to the development of Mondor’s Disease.
- Hypercoagulable state: Conditions that increase the tendency for blood to clot may be associated with an increased risk of developing Mondor’s Disease.
Importance of Awareness and Early Detection
While Mondor’s Disease is a relatively rare condition, being aware of the symptoms and risk factors is crucial for timely diagnosis and appropriate management. Early detection can help prevent complications and ensure prompt treatment. If you experience any concerning symptoms or have a family history of Mondor’s Disease, it is recommended to consult with a healthcare professional for further evaluation.
Prevalence of Mondor’s Disease in Women and Men
| Population | Prevalence in Women | Prevalence in Men |
|---|---|---|
| General Population | Unknown | Unknown |
| Specific Subgroups | Varies | Varies |
Note: Due to the rarity of Mondor’s Disease and the limited available data, the exact prevalence rates in women and men are not well-established and may vary across different populations.
Surgical Options for Mondor’s Disease
In rare cases where conservative measures are not effective, surgical intervention may be considered for Mondor’s Disease, including penile Mondor’s disease. Surgical options for the treatment of Mondor’s Disease involve removing the blood clot and resecting the affected vein.
The first surgical choice is thrombectomy, where the goal is to remove the blood clot causing issues in the affected vein. This helps bring back normal blood flow and eases symptoms like pain and swelling.
Another option is resection, where the damaged vein is entirely removed. This might be considered if the vein is severely damaged or if other treatments don’t work.
Both thrombectomy and resection can often be done on an outpatient basis, meaning patients can go home the same day. The recovery period for these surgeries is typically around eight weeks, and patients may need to follow specific post-surgery care instructions from their healthcare providers.
In summary, although most Mondor’s Disease cases can be treated without surgery, there are situations where surgery might be needed. Thrombectomy and resection are two surgical options to address Mondor’s Disease by removing the blood clot and the affected vein. People considering surgery should consult with their healthcare professionals to discuss the procedure’s risks, benefits, and potential outcomes.
In the context of Mondor’s Disease, it’s important to note that this rare condition, more common in women and often showing a subcutaneous cord, underscores the significance of considering a patient’s medical history when assessing symptoms. Accessing information through the official website ensures secure data transmission, adhering to a creative commons attribution-noncommercial-noderivatives 4.0 international license.
Because of its rarity, a thorough examination, including imaging studies like ultrasound, is crucial for an accurate diagnosis. This diagnostic approach is especially important when there’s no flow signal, contributing to understanding and effectively managing Mondor’s Disease. Recognizing these features, even within a week before symptoms appear, is vital for a timely and secure diagnosis of this unique medical condition involving the thoracic wall.
MONDOR DISEASE OF THE BREAST
Mondor’s disease of the breast, also known as Mondor’s syndrome, is a rare and generally benign condition characterized by inflammation of the superficial veins in the breast and the surrounding chest wall. Named after the French surgeon Henri Mondor, this condition typically presents as painful cord-like structures under the skin, which are actually thrombosed or clotted veins.
Key points about Mondor’s disease of the breast:
- Symptoms: The main symptom is the presence of tender, palpable cords or bands in the breast or chest wall. Pain may increase with movement or palpation.
- Cause: The exact cause of Mondor’s disease is not always clear, but it is often associated with trauma, surgery, or inflammation in the chest or breast area.
- Diagnosis: Clinical examination and medical history are usually sufficient for diagnosis. Imaging studies like ultrasound may be used to rule out other conditions.
- Treatment: Mondor’s disease is generally self-limiting, and symptoms may resolve on their own over time. Pain relief measures, such as nonsteroidal anti-inflammatory drugs (NSAIDs), may be recommended. Severe cases may require additional medical intervention.
- Prognosis: Mondor’s disease is considered a benign and self-limiting condition. The prognosis is generally favorable, with most cases resolving without long-term complications.
Also Read : Top Ways To Avoid Common Medical Problems
Conclusion
Mondor’s Disease, including penile Mondor’s disease, is a rare vascular condition characterized by thrombophlebitis in the superficial veins. This condition can present with various symptoms such as pain, swelling, and palpable hardened veins. Through physical examination and imaging tests, such as ultrasound, healthcare professionals can diagnose Mondor’s Disease accurately.
Treatment for this rare vascular condition is primarily supportive, aiming to relieve pain and inflammation. Patients are advised to abstain from sexual activity until the symptoms resolve to avoid further irritation and prolongation of the healing process. In the majority of cases, Mondor’s disease resolves on its own within four to six weeks without any complications.
While complications are rare, it is essential to monitor for any signs of deep vein thrombosis (DVT), such as persistent pain, swelling, or warmth in the affected area. If any symptoms occur, seeking medical attention is crucial to ensure timely diagnosis and appropriate management.
In conclusion, Mondor’s Disease is a rare vascular condition that requires prompt diagnosis and appropriate treatment for symptom management. With early intervention and proper care, the prognosis for individuals with Mondor’s Disease, including penile Mondor’s disease, is generally favorable.
FAQs
What is Mondor’s disease?
Mondor’s disease, also known as superficial thrombophlebitis of the breast, is a rare condition characterized by inflammation and thrombosis of the subcutaneous veins of the anterior chest wall.
What are the symptoms of Mondor’s disease?
Symptoms of Mondor’s disease include a palpable cord-like induration, skin retraction, and pain or tenderness in the affected area.
What are the causes of Mondor’s disease?
A: The exact cause of Mondor’s disease is not fully understood, but it is often associated with underlying diseases, trauma, or surgery, such as aesthetic breast surgery.
How is Mondor’s disease diagnosed?
A: Diagnosis of Mondor’s disease is usually based on clinical examination and medical history. Imaging studies, such as ultrasound and mammography, may also be used to confirm the diagnosis.
What treatment options are available for Mondor’s disease?
Treatment for Mondor’s disease may include pain management, anti-inflammatory medications, and in some cases, anticoagulant therapy. In severe cases, surgical intervention may be necessary.
Is Mondor’s disease associated with breast cancer?
Mondor’s disease is not directly associated with breast cancer, but it has been reported in association with breast cancer, especially in cases of aggressive breast cancer.
What is Penile Mondor’s disease?
Penile Mondor’s disease is a rare condition that affects the superficial penile veins, causing pain, swelling, and a palpable cord-like structure on the penile shaft.